Abstract
Introduction Donor T-cell recognition of tumor-presented minor histocompatibility antigens (mHAs) is thought to be a central mediator of the therapeutic graft versus leukemia (GvL) effect following allogeneic hematopoietic cell transplantation (alloHCT). In contrast, graft versus host disease (GvHD) develops when donor T-cells react to mHAs presented by normal recipient cells. While the role of mHAs in outcomes following alloHCT is recognized, it has not been well-characterized. It remains unclear whether GvL and GvHD are mediated by the cumulative effect of total mHAs in a donor-recipient pair (DRP) or individual immunodominant mHAs.
We hypothesized that an increased mHA count and individual mHAs would be associated with lower relapse and disease-related mortality (DRM) and/or increased GvHD mortality. To this end, we predicted genome-wide mHA peptides in a large patient population and analyzed the associations between clinical outcomes and 1) the total number of predicted class I and class II mHAs, and (2) individual and groups of mHAs.
Methods The study population consisted of 2249 European American DRPs in the DISCOVeRY-BMT dataset treated for Acute Myeloid Leukemia (AML) and Myelodysplastic Syndrome (MDS) with alloHCT. To predict mHAs in a DRP, we translated nonsynonymous SNP alleles present in alloHCT recipients, but absent in their donor, into all possible peptides of varying lengths that would encompass the altered amino acid. To identify mHAs most likely to be immunogenic, peptides were filtered based on (1) source protein gene expression data in GvL and GvHD target tissues, including AML, liver, skin, and colon, from UCSC's Xena Dataset repository and (2) recipient HLA binding affinity from netMHCpan.
To test the association of mHA count and individual mHAs with all-cause mortality (OS) and leukemia-free survival (LFS) we used cox proportional hazard models and competing risk models for DRM, treatment-related mortality (TRM), and GvHD mortality. Individual mHA analyses were stratified by HLA type to recognize that T-cell responses depend on HLA-mHA complexes. Models were adjusted for clinical covariates. Bonferroni correction for multiple testing was based on the number of independent SNPs.
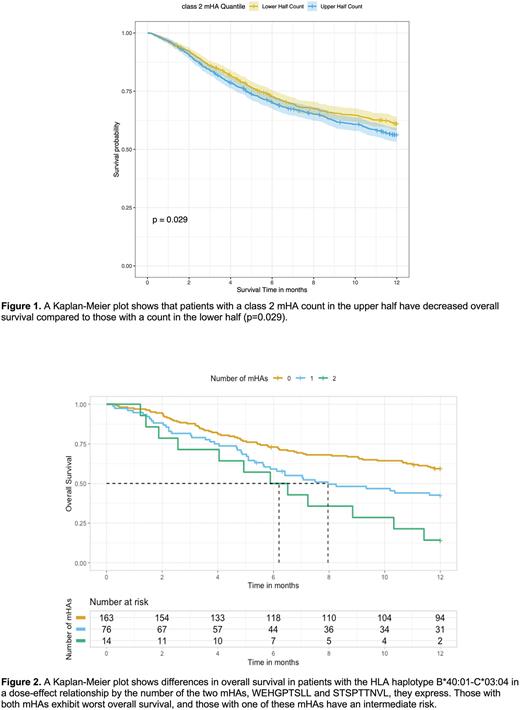
Results Patients with a class I mHA count greater than the population median had a 39% (HR=1.39, 95%CI 1.005,1.772, P=0.046) increase in hazard of GvHD mortality compared to those with a count less than the median. Patients with a class II mHA count greater than the population median had a decreased overall survival compared to those with a count less than the median (Fig. 1, P=0.029).
In recipients with HLA-B*08:01, the class I mHA DLRCKYISL was associated with increased risk of GVHD mortality (HR=2.84, 95%CI 1.52,5.31, P=0.01). Within HLA-B*40:01, WEHGPTSLL was associated with decreased LFS (HR=1.94, 95%CI 1.27,2.95, P=0.044). Within HLA-C*03:04, STSPTTNVL was associated with increased risk of DRM (HR=2.32, 95%CI 1.5,3.6, P=0.008). In recipients with HLA-DRB1*15:01, the class II mHA YQEIAAIPSAGRERQ was associated with increased risk of TRM (HR=3.05, 95%CI 1.75,5.31, P=0.02).
Two mHAs, WEHGPTSLL and STSPTTNVL, were found within the HLA haplotype B*40:01-C*03:04. Recipients with both mHAs (versus neither) had a greater hazard of 1-year all-cause mortality (HR=3.58, P=7.9×10-5) and DRM (HR=3.65, P=0.003) (Fig. 2). Patients with either mHA (versus neither) had greater 1-year all-cause mortality (HR=1.69, P=0.008) and increased DRM (HR=2.05, P=0.008)
Conclusions The number of class I mHAs in a DRP was associated with increased GvHD mortality, which is consistent with our hypothesis. We also found two mHAs correlated with GvHD mortality and DRM which may represent increased GvH effects driven by these peptides.
However, contrary to our hypothesis, an increased number of class II mHAs was correlated with greater risk of all-cause mortality that may be due to decreased LFS. Similarly, we found two mHAs correlated with increased DRM and decreased LFS. These two mHAs are found in an HLA haplotype where they exhibit a dose effect relationship with the risk of DRM and decreased OS. These findings may reflect an unexpectedly attenuated GvL effect that requires further investigation.
Our study reports the first large scale investigation of the role of predicted mHA peptides in clinical outcomes following alloHCT. If validated, these results may be used to help guide clinical decision making.
Disclosures
Pasquini:Kite: Research Funding; Bristol Myers Squibb: Consultancy, Research Funding; Janssen: Research Funding; Novartis: Research Funding. McCarthy:Bristol Myers Squibb Company: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Consultancy, Honoraria; Janssen Global Services, LLC: Consultancy, Honoraria; Karyopharm Therapeutics Inc.: Consultancy, Honoraria; Partner Therapeutics, Inc.: Consultancy, Honoraria; Axios: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda Pharmaceuticals America, Inc.: Consultancy, Honoraria; Fate Therapeutics: Consultancy, Honoraria; Magenta Therapeutics: Consultancy, Honoraria; Oncopeptides: Consultancy, Honoraria; Juno: Consultancy, Honoraria; Bluebird Bio: Consultancy, Honoraria; Sanofi: Consultancy; Starton Therapeutics: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria. Sucheston-Campbell:Roche: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal